- 29 January 2024
- 153
Talking about Tumors: How Insulinoma Affects Blood Sugar
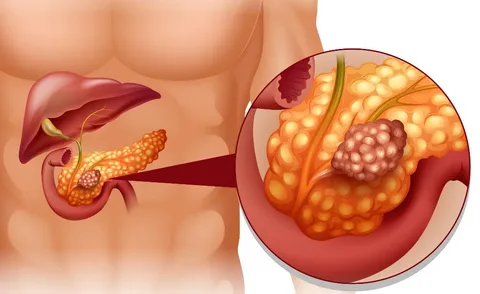
What Is an Insulinoma?
Insulinomas, a rare subtype of pancreatic tumors, originate from beta islet cells responsible for insulin secretion. Unlike the typical pancreatic response to blood sugar levels, insulinomas lead to persistent insulin production, causing continuous low blood sugar.
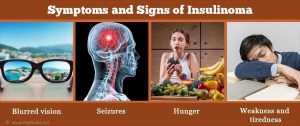
Insulinoma Symptoms in Points
Identifying insulinoma symptoms is crucial for early detection. The condition manifests through:
- Confusion: Mental fog or disorientation
- Sweating: Profuse perspiration, especially during non-strenuous activities
- Weakness: Generalized fatigue and lack of energy
- Anxiety: Elevated feelings of nervousness
- Fast Heartbeat: Increased heart rate unrelated to physical exertion
- Headache: Persistent or severe headaches
- Vision Changes: Altered visual perception
- Personality Changes: Shifts in behavioral traits
- Crankiness: Irritability and mood swings
- Lack of Muscle Coordination: Difficulty in coordinating movements
- Blurred Vision: Impaired visual clarity
- Lethargy: Persistent fatigue
- Seizure: Uncontrolled muscle contractions
- Pale Appearance (Pallor): Unusual paleness
These symptoms, if left unaddressed, may progress to severe complications such as fainting or coma due to dangerously low blood sugar levels.
Causes and Risk Factors
The etiology of insulinomas remains elusive, though they exhibit a higher prevalence in women aged 40-60. Individuals with specific genetic conditions, including multiple endocrine neoplasia type 1, Von Hippel-Lindau syndrome, neurofibromatosis type 1, and tuberous sclerosis, are at an elevated risk.

Diagnosis
Diagnosing insulinomas is a complex process due to symptom overlap with other health issues. Comprehensive tests are conducted, including:
- Blood tests and Suppression Tests: Assessing blood sugar, insulin, C-peptide, and proinsulin during a 72-hour fast to confirm low blood sugar symptoms.
- Imaging Tests: CT scans, ultrasounds, or MRIs to locate the tumor within the pancreas.

Treatments
The primary treatment for insulinomas is surgical intervention, aiming to remove the tumor and achieve a cure. Surgical approaches include traditional and laparoscopic methods. Laparoscopic surgery, a minimally invasive option, ensures reduced pain, shorter hospital stays, and faster recovery. In cases where surgery is deemed impractical, managing low blood sugar through medication and dietary adjustments becomes pivotal.
Treatment for Cancerous Insulinomas
In rare instances where insulinomas are cancerous, alternative treatments may be explored. Options include chemotherapy or lutetium Lu 177 dotatate (Lutathera), a radioactive medicine that selectively targets tumor cells.
Complications
While surgery is often curative, potential complications may include:
- Bleeding
- Infection
- Pain
- High Blood Sugar (Diabetes)
- Pancreatic Fistula
- Low Digestive Enzymes
Understanding these potential complications underscores the importance of postoperative monitoring and care. Treatment For other Health Problems
Comparative Table: Surgery vs. Non-Surgical Treatments
| Aspect | Surgery | Non-Surgical Treatments |
|---|---|---|
| Primary Approach | Tumor removal from pancreas | Medication, dietary adjustments |
| Procedure Type | Laparoscopic or traditional | Medication management, lifestyle |
| Cure Rate | High | Symptomatic relief, not curative |
| Complications | Bleeding, infection, pain | Medication side effects, dietary |
Understanding the multifaceted nature of insulinomas is paramount for informed decision-making and personalized treatment plans. Individuals experiencing symptoms are urged to consult healthcare professionals promptly for accurate diagnosis and tailored interventions.

