- 12 January 2024
- 719
Preventing Diabetic Kidney Disease
Introduction
The intricate relationship between diabetes and kidney health unveils a complex scenario where the kidneys, vital organs responsible for filtering waste and excess fluid, become susceptible to disease in individuals grappling with diabetes. In this article, we delve into the multifaceted aspects of Diabetic Kidney Disease (DKD), exploring its nuances, symptoms, diagnostic procedures, and comprehensive treatment strategies.
Understanding Diabetic Kidney Disease
What is Diabetic Kidney Disease?
Diabetic Kidney Disease, or diabetic nephropathy, manifests as a complication in some individuals with diabetes. The crux of the matter lies in the damage inflicted upon the kidney filters, known as glomeruli, resulting in abnormal protein leakage, notably albumin, from the bloodstream into the urine.
Categories of Diabetic Kidney Disease
- Microalbuminuria: In this stage, albumin leakage ranges from 30 to 300 mg per day.
- Proteinuria: This more severe stage involves albumin leakage exceeding 300 mg per day, often termed macroalbuminuria or overt nephropathy.

Development and Progression
The elevation of blood sugar levels in diabetes triggers chemical changes in the kidneys, rendering glomeruli more permeable. This increased permeability allows albumin to seep into the urine, initiating a scarring process termed glomerulosclerosis. This gradual process, occurring over several years, can lead to a decline in kidney function, eventually culminating in end-stage kidney failure.
Prevalence
Diabetic kidney disease exhibits a higher prevalence in type 2 diabetes, primarily due to the higher incidence of this type of diabetes. Notably, it stands as the leading cause of kidney failure, impacting approximately one in five individuals requiring dialysis.
Symptoms
Symptoms of early diabetic kidney disease, especially during the microalbuminuria stage, may not be overt. However, as the disease progresses, symptoms can become more pronounced and include:
- Difficulty thinking clearly
- Poor appetite
- Weight loss
- Dry, itchy skin
- Muscle cramps
- Fluid retention leading to swollen feet and ankles
- Puffiness around the eyes
- Increased frequency of urination
- Paleness due to anemia
- Nausea
Diagnosis and Assessment
Diagnosis involves routine urine tests measuring albumin levels and blood tests assessing kidney function. The albumin:creatinine ratio (ACR) in urine samples and the estimated glomerular filtration rate (eGFR) from blood tests are crucial parameters.
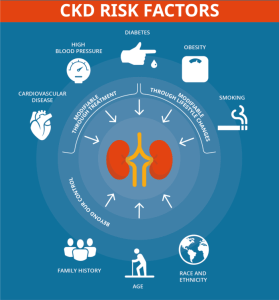
Risk Factors
Certain factors increase the risk of developing diabetic kidney disease:
- Poor control of blood sugar levels
- Duration of diabetes
- Weight gain
- High blood pressure
- Gender (more prevalent in males)
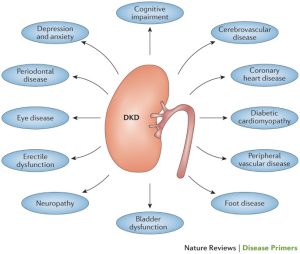
Complications
End-Stage Kidney Failure
In individuals with proteinuria, end-stage kidney failure may develop in approximately 1 in 12 people after 10 years, necessitating kidney dialysis or transplant.
Cardiovascular Diseases
All individuals with diabetes face an increased risk of cardiovascular diseases, with diabetic kidney disease amplifying this risk. The severity of kidney disease directly correlates with the heightened cardiovascular risk.
High Blood Pressure
Kidney disease and high blood pressure often create a detrimental cycle. High blood pressure exacerbates kidney disease, and kidney disease contributes to increased blood pressure. Managing blood pressure becomes a pivotal aspect of treating diabetic kidney disease.
Treatment Strategies
Medications
- ACE Inhibitors: These medications reduce the production of angiotensin II, a chemical narrowing blood vessels, aiding in blood pressure regulation and offering protective effects on the kidneys.
- Angiotensin-II Receptor Antagonists (AIIRA): These work similarly to ACE inhibitors and may be an alternative if side effects occur.
Additional Medication
- Finerenone: Recommended by NICE, this medication works differently from ACE inhibitors and AIIRAs.

Lifestyle Modifications
- Blood Glucose Control: Maintaining optimal blood sugar levels delays kidney disease progression and reduces cardiovascular disease risk.
- Blood Pressure Management: Strict blood pressure control is crucial, often involving ACE inhibitors or AIIRAs. Additional medications may be prescribed if blood pressure remains elevated.
- Cholesterol Level Management: Medications to lower cholesterol levels help mitigate the risk of complications like heart disease, peripheral arterial disease, and stroke.
- Lifestyle Adjustments: Quitting smoking, adopting a healthy diet, weight management, regular physical activity, and alcohol moderation contribute to overall kidney health.

Outlook
Microalbuminuria
This stage may improve with treatment, especially if managed promptly.
Proteinuria
Over time, proteinuria tends to progress, potentially leading to end-stage kidney failure. The progression rate varies, and timely referral to a kidney specialist becomes imperative.
Cardiovascular Disease Risk
Cardiovascular diseases, particularly heart attack and stroke, pose significant threats to individuals with diabetic kidney disease. Comprehensive treatments outlined above aim to reduce these risks, emphasizing the holistic approach needed in managing this complex condition.
Conclusion
In navigating the complex landscape of Diabetic Kidney Disease (DKD), it becomes evident that a proactive approach is essential. Early detection through routine tests, meticulous management of blood sugar and pressure, and a multifaceted treatment strategy contribute to better outcomes. While complications like end-stage kidney failure and heightened cardiovascular risks loom, comprehensive lifestyle adjustments and advancements in medication provide hope. The synergy between medical intervention and individual commitment becomes the cornerstone for effectively tackling DKD.

