- 17 April 2023
- 137
Beyond Chemotherapy: Exploring the Emerging Frontier of Cancer Vaccines
Cancer has been a devastating disease for decades, affecting millions of lives around the world. While chemotherapy and radiation therapy have been the traditional methods used to fight cancer, recent advancements in medical science have opened up new frontiers in cancer treatment. Cancer vaccines offer an innovative approach that can potentially revolutionize cancer treatment as we know it. In this blog post, we will explore the emerging frontier of cancer vaccines- what they are, how they work, their safety and effectiveness levels, types of cancers that can be treated with them, clinical trials and FDA-approved cancer vaccines. So fasten your seat belts as we take you on an exciting journey into this cutting-edge field!
What are cancer vaccines?
Cancer vaccines are a type of immunotherapy that targets cancer cells in the body. Unlike traditional vaccines that prevent infections, cancer vaccines aim to stimulate the immune system to recognize and attack cancer cells. These vaccines may contain substances called antigens derived from cancer cells or DNA fragments specific to the tumor.
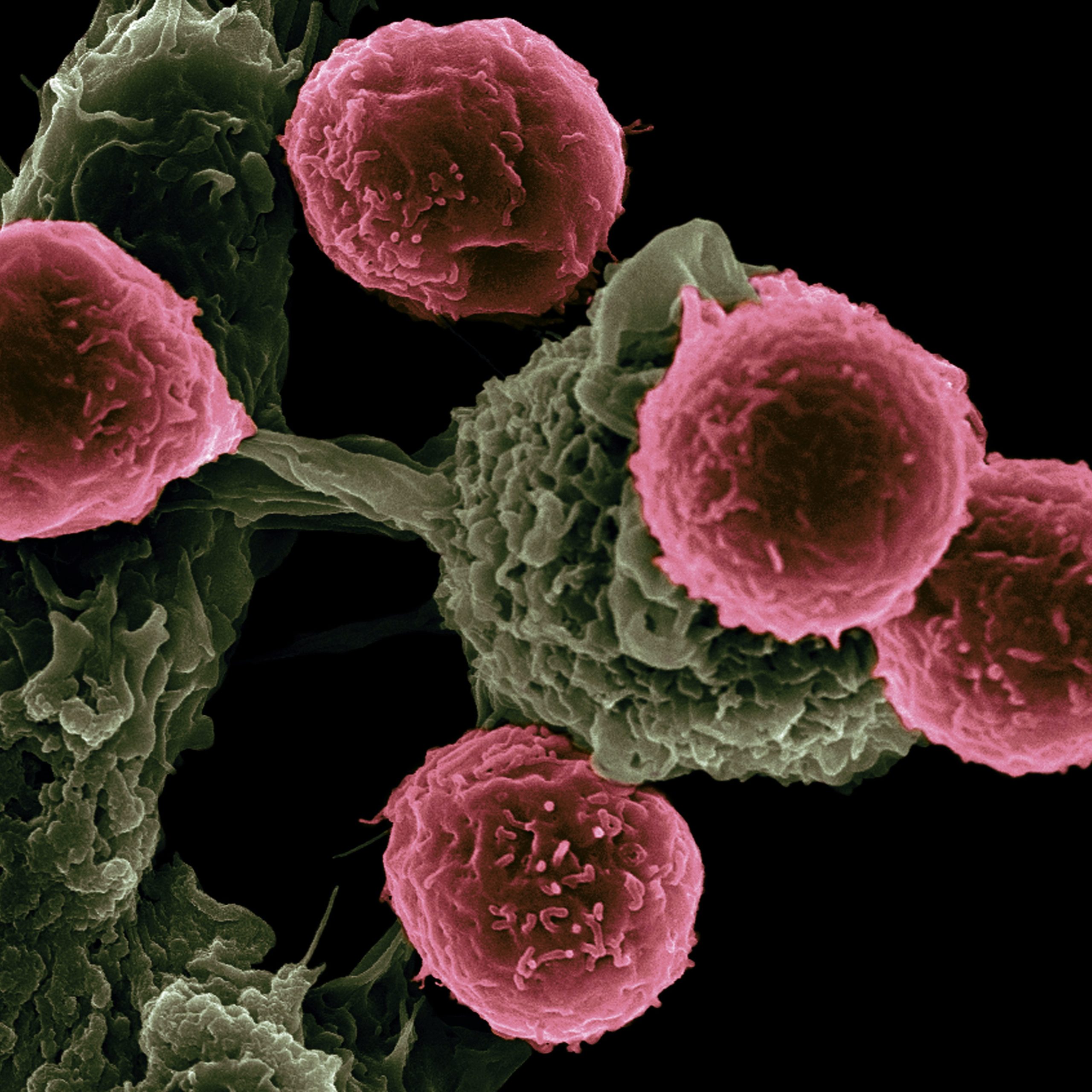
When injected into the body, these antigens trigger an immune response which activates the white blood cells known as T-cells and B-cells. These specialized cells then scavenge through the bloodstream searching for malignant cells with similar antigen structures, in turn killing them off.
Some types of cancer vaccines can also be used to prevent certain cancers by boosting immunity against viruses associated with some cancers such as human papillomavirus (HPV).
While still in experimental stages, researchers believe that this treatment option could potentially be less toxic than other forms of therapy and offer long-term protection against recurrence.
How do cancer vaccines work?
Cancer vaccines work by stimulating the immune system to recognize and attack cancer cells. Unlike traditional vaccines that prevent viral or bacterial infections, cancer vaccines are designed to treat existing cancers.
One type of cancer vaccine is called a tumor-specific antigen vaccine. These vaccines contain proteins found only on the surface of certain types of cancer cells. When injected into the body, these proteins trigger an immune response that targets and destroys those specific cancer cells.
Another type of cancer vaccine is known as a dendritic cell vaccine. Dendritic cells are immune cells that play a key role in activating other parts of the immune system. In this type of vaccine, dendritic cells are extracted from the patient’s blood and exposed to tumor antigens in a lab setting before being injected back into the patient’s body. The activated dendritic cells then stimulate an immune response against any remaining cancerous tissue.
Cancer vaccines can also be combined with other treatments such as chemotherapy or radiation therapy for maximum effectiveness. While still considered an emerging field with ongoing research, early studies have shown promising results for some types of cancers including melanoma and prostate cancer.
While there is still much to learn about how exactly immunotherapy works, it has become clear that harnessing our own bodies’ natural defenses may hold great potential for treating even some of the most aggressive forms of malignancies.
Are cancer vaccines safe?
Cancer vaccines have been a topic of discussion for many years, but some may wonder if they are safe to use. It’s important to note that cancer vaccines are different than traditional vaccines as they do not prevent illnesses, but rather aim to treat existing conditions.
One type of cancer vaccine is the therapeutic vaccine which helps train your immune system to fight against cancer cells. This process works by using specific proteins found in certain cancers and combining them with substances called adjuvants, which help stimulate the immune response.
Another type is called the preventive or prophylactic vaccine, which aims at preventing certain types of cancers caused by viruses such as human papillomavirus (HPV) or hepatitis B virus (HBV).
While there are concerns about the safety of these vaccines, studies have shown them to be generally well-tolerated with only mild side effects such as fatigue, headache and fever. Serious adverse reactions are rare.
It’s important for individuals interested in receiving a cancer vaccine to consult their healthcare provider before doing so. They can provide more information on individual risks and benefits based on medical history and current health status.
While no medical intervention is completely risk-free, current evidence suggests that cancer vaccines offer promising potential with relatively low risks compared to other treatment options.
What are the side effects of cancer vaccines?
As with any medical treatment, cancer vaccines can cause side effects. However, the side effects of cancer vaccines are generally mild and well-tolerated.
The most common side effects of cancer vaccines include pain, redness, or swelling at the injection site. Some people may also experience fever, fatigue, and headache for a few days after receiving the vaccine.
In rare cases, more serious side effects such as an allergic reaction or severe inflammation may occur. It’s important to talk to your doctor if you experience any concerning symptoms after receiving a cancer vaccine.
It’s worth noting that because cancer vaccines work by stimulating the immune system, some people may mistakenly believe that they have developed a new tumor when experiencing immune-related symptoms like enlarged lymph nodes or skin rashes. However, these symptoms are often signs that the vaccine is working as intended.
While there is always a risk of side effects with any medical treatment including cancer vaccines; these potential risks should be weighed against the potential benefits of preventing and treating this deadly disease.
How effective are cancer vaccines?
Cancer vaccines have shown promise in clinical trials, with some showing significant effectiveness. However, the effectiveness of cancer vaccines can vary depending on several factors.
Firstly, the type and stage of cancer being treated can affect how effective a vaccine is. Vaccines are more likely to be effective against early-stage cancers that haven’t spread throughout the body.
Secondly, a person’s immune system plays a crucial role in determining the effectiveness of a cancer vaccine. If a person has a weakened immune system or an existing condition that affects their immunity, they may not respond as well to treatment.
Like with any medical intervention, there are no guarantees when it comes to cancer vaccines. Some people may experience little benefit while others see significant improvements in their condition.
While there is still much research needed to fully understand how effective cancer vaccines can be for different types and stages of cancer patients – they offer hope for individuals who have previously had limited options for treatment.
What types of cancer can be treated with vaccines?
Cancer vaccines have shown promise in treating a variety of cancers, including melanoma, prostate cancer, and lung cancer. One type of vaccine targets antigens specific to the patient’s tumor cells. Another approach is to use a virus or bacteria that has been modified to carry cancer-specific proteins.
Melanoma is one of the most aggressive types of skin cancer and accounts for the majority of skin-related deaths. Cancer vaccines have been successful in treating late-stage melanoma by targeting specific proteins found on the surface of these tumors.
Prostate cancer is another common form of cancer that can be treated using vaccines. The FDA approved Provenge, a therapeutic vaccine for advanced prostate cancer in 2010.
Lung cancer is also being studied as a potential target for vaccination therapy. Researchers are testing whether combining immune checkpoint inhibitors with vaccines could improve treatment outcomes.
While more research needs to be done into what types of cancers can benefit from vaccination therapy, there are promising results showing that it may offer hope for patients with various forms of this disease.
Clinical trials for cancer vaccines
Clinical trials are an essential part of cancer vaccine research. These trials aim to test the safety and efficacy of cancer vaccines before they can be approved for use in patients. Typically, clinical trials involve a small group of volunteers who meet specific eligibility criteria.
During clinical trials, participants receive doses of the vaccine over a specified period. Doctors closely monitor each participant’s health to detect any adverse reactions or side effects resulting from the vaccine’s administration.
The initial goal of these clinical trials is to determine whether the vaccine is safe for human use. Once researchers confirm its safety profile, they will begin testing whether it has any therapeutic effect on cancer cells.
In some cases, these clinical studies may include comparing treatments already in use with new vaccines undergoing evaluation. This comparison aims to establish if one treatment option is better than another in terms of their effectiveness against particular types of cancers.
It should be noted that not all vaccines tested during clinical trials become FDA-approved or widely used by doctors as standard treatment options for certain cancers. Instead, many are still being studied and improved upon through continued research efforts.
FDA-approved cancer vaccines
FDA-approved cancer vaccines are a significant step in the field of immunotherapy. These vaccines have undergone rigorous testing and clinical trials to prove their safety and effectiveness.
One such vaccine is Gardasil, which was originally approved for the prevention of human papillomavirus (HPV) that can lead to cervical cancer. It has since been found effective in preventing other types of cancers caused by HPV.
Another FDA-approved cancer vaccine is Provenge, which stimulates the immune system to attack prostate cancer cells. This personalized treatment uses a patient’s own white blood cells that have been “trained” to target specific proteins found on prostate cancer cells.
In 2020, Tecentriq became the first FDA-approved immunotherapy drug for non-small cell lung cancer (NSCLC). This medication works by blocking PD-1/PD-L1 interactions between tumors and immune cells, allowing the immune system to better recognize and attack NSCLC cells.
These FDA-approved vaccines provide hope for patients with various forms of cancers. As research continues, it is likely we will see more breakthroughs in this exciting area of medicine.
Cancer vaccine research
Cancer vaccine research is an active area of study in the field of oncology. Researchers are trying to develop vaccines that can help prevent cancer or treat it more effectively. One approach being explored involves using a patient’s own immune system to recognize and attack cancer cells.
There are several different types of cancer vaccines under investigation, including peptide-based vaccines, DNA-based vaccines, and whole-cell vaccines. These approaches involve introducing specific molecules from cancer cells into the body in order to stimulate an immune response against them.
One challenge with developing effective cancer vaccines is that tumors can often evade detection by the immune system or suppress its activity. Researchers are exploring ways to overcome these obstacles through techniques such as combining vaccine treatments with other therapies like checkpoint inhibitors.
Another important focus of cancer vaccine research is identifying which patients will benefit most from vaccination. This may involve studying genetic markers or tumor characteristics that can predict a patient’s response to treatment.
While there have been some promising results from early clinical trials of cancer vaccines, more research is needed before they become widely available for use in treating patients with various forms of this disease.
Conclusion
Cancer vaccines represent a promising frontier in the fight against cancer. While chemotherapy and radiation therapy have been effective for many patients, they are often associated with significant side effects and limitations. Cancer vaccines offer a more targeted approach that can stimulate the body’s immune system to attack cancer cells specifically.
Clinical trials of these vaccines have shown promising results, with some demonstrating significant improvements in survival rates for patients with certain types of cancers. The FDA has also approved several cancer vaccines for use in specific contexts.
While there is still much work to be done before cancer vaccines become widely available as a treatment option, ongoing research continues to show promise. As we learn more about how different cancers interact with the immune system, it is likely that new approaches will emerge that could further improve outcomes for patients.
Cancer vaccine development represents an exciting avenue of research that holds great potential for improving patient outcomes and reducing the burden of this devastating disease on individuals and society as a whole.

