- 8 January 2024
- 264
Alcohol and the Liver: Unveiling Alcoholic Hepatitis Risks and Protective Actions
Understanding Alcoholic Hepatitis
Alcoholic hepatitis is a condition characterized by inflammation of the liver due to excessive alcohol consumption. The liver is a vital organ responsible for processing and metabolizing substances, including alcohol. When alcohol is consumed in large amounts over an extended period, it can lead to liver damage and inflammation.
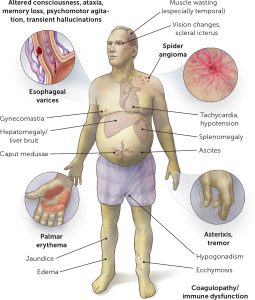
Common Signs And Symptoms
Common Signs and Symptoms Normal Drinkers
- Abdominal Pain and Tenderness: Pain and discomfort in the abdominal area, especially around the liver.
- Nausea and Vomiting: Individuals with alcoholic hepatitis may experience persistent nausea and vomiting.
- Fatigue: Feeling extremely tired and weak, even with minimal physical activity.
- Loss of Appetite: A decrease in the desire to eat, which can lead to weight loss.
- Fever: Some people with alcoholic hepatitis may develop a fever.
- Ascites: Accumulation of fluid in the abdominal cavity, leading to abdominal swelling.
Symptoms In Heavy Drinkers
People with alcoholic hepatitis tend to be malnourished. Drinking large amounts of alcohol keeps people from being hungry. And heavy drinkers get most of their calories from alcohol.
Other symptoms that happen with severe alcoholic hepatitis include:
- Fluid buildup in the belly, called ascites.
- Being confused and acting oddly due to a buildup of toxins. The healthy liver breaks these toxins down and gets rid of them.
- Kidney and liver failure.
Causes
These factors are known to play a role in alcoholic hepatitis:
-
- The body’s way of breaking down alcohol makes highly toxic chemicals.
- These chemicals trigger swelling, called inflammation, that destroys liver cells.
- Over time, scars replace healthy liver tissue. This keeps the liver from working well.
- This scarring, called cirrhosis, can’t be fixed. It’s the final stage of alcoholic liver disease.
Other factors that can be involved with alcoholic hepatitis include:
- Other types of liver disease. Alcoholic hepatitis can make chronic liver diseases worse. For instance, if you have hepatitis C and drink, even a little, you’re more likely to get liver scarring than if you don’t drink.
- Lack of nutrition. Many people who drink heavily don’t get enough nutrients because they eat poorly. And alcohol keeps the body from using nutrients as it should. Lack of nutrients can damage liver cells.

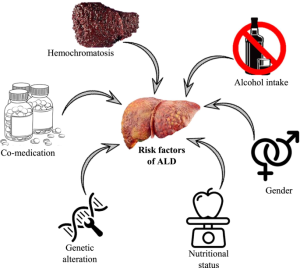
Risk Factors
The major risk factor for alcoholic hepatitis is the how much alcohol you drink. It isn’t known how much alcohol it takes to cause alcoholic hepatitis.
Most people with this condition have had at least seven drinks a day for 20 years or more. This can mean 7 glasses of wine, 7 beers, or 7 shots of spirits.
However, alcoholic hepatitis can happen to people who drink less and have other risk factors, including:
- Sex. Women seem to have a higher risk of getting alcoholic hepatitis. That might be because of how alcohol breaks down in women’s bodies.
- Obesity. Heavy drinkers who are overweight might be more likely to get alcoholic hepatitis. And they might be more likely to go on to get liver scarring.
- Genes. Studies suggest that genes might be involved in alcohol-induced liver disease.
- Race and ethnicity. Black and Hispanic people might be at higher risk of alcoholic hepatitis.
- Binge drinking. Having five or more drinks in about two hours for men and four or more for women might increase the risk of alcoholic hepatitis.
Complications
Alcoholic hepatitis can lead to various complications, especially if the condition is severe and not properly managed. Some of the complications associated with alcoholic hepatitis include:
- Liver Cirrhosis: Alcoholic hepatitis is a significant risk factor for the development of liver cirrhosis. Cirrhosis is characterized by the formation of scar tissue in the liver, which can impair liver function over time. Cirrhosis is a progressive and irreversible condition.
- Liver Failure: In severe cases of alcoholic hepatitis, the liver may lose its ability to function properly, leading to liver failure. Liver failure is a life-threatening condition requiring immediate medical attention.
- Portal Hypertension: Liver damage can result in increased pressure in the portal vein, the major blood vessel that carries blood from the digestive organs to the liver. This condition is known as portal hypertension and can lead to complications such as varices (enlarged veins) in the esophagus and stomach, which may rupture and cause severe bleeding.
- Ascites: Accumulation of fluid in the abdominal cavity is common in advanced liver disease. Ascites can lead to abdominal swelling and discomfort.
- Hepatic Encephalopathy: Liver dysfunction can lead to the buildup of toxins in the blood, affecting brain function. Hepatic encephalopathy can result in confusion, altered consciousness, and in severe cases, coma.
- Kidney Dysfunction: Liver failure can impact kidney function, leading to a condition known as hepatorenal syndrome. This can result in kidney failure.
- Increased Risk of Infections: Weakened immune function due to liver damage increases the risk of infections, which can further complicate the clinical picture.
- Increased Risk of Bleeding Disorders: Liver dysfunction can affect the production of clotting factors, leading to an increased risk of bleeding disorders.